United Health Care Community Plan Prior Authorization
Integrity of Claims Reports and Representations to the Government UnitedHealth Group requires compliance with the requirements of federal and state laws that prohibit the submission of false claims in connection with federal health care programs including Medicare and Medicaid. Provider resources for UnitedHealthcare Community Plan of North Carolina products including prior authorization information provider manuals forms recent news and more.

Policy 16 1 Structural Facilitators And Barriers To Access To And Continuity Of Healthcare Health Care Policy Social Services French Language
UnitedHealthcare requires that care providers complete the notificationprior authorization process for genetic and molecular testing performed in an outpatient setting for UnitedHealthcare Community Plan members in these states.

United health care community plan prior authorization. You do not need prior authorization for emergencies or to go to an urgent care center. More than half of the prior authorizations we receive each month are through electronic prior authorization ePA. 1 2019 Opens in a new window open_in_new.
We use prior authorization concurrent review and post-review to ensure appropriateness medical need and efficiency of health care services. Many practices however remain unaware of the benefits that ePA offers. UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program.
Beginning March 1 2019. If a prior authorization is denied you. Prior Authorization Required All nursing facility services require authorization.
This is called prior authorization. Provider resources for Michigan Community Plan products including prior authorization information provider manuals forms recent news and more. This is called a prior authorization.
1 2017 notification is required for certain genetic and molecular lab tests for certain UnitedHealthcare Commercial benefit plans. 711 Hearing Impaired Fax. Persons covered under a UnitedHealthcare Community Plan UHC have access to a wide range of prescription medication.
If a prior authorization is approved those services will be covered by your health plan. 87726 EDI Claims Submission For ERA use Payer ID 04567 Behavioral Health Services Information Call Center. UnitedHealthcare Senior Care Options HMO SNP Plan.
Your PCP or Doctor will work with us to get prior authorization if needed. Provider - ePA saves administrative time by making it easier to submit and track prior authorizations and enables faster. Prior Authorization Requirements for Certain Therapy Services - Effective Oct.
In some cases an approval is needed from your health plan before some health care services will be covered. The purpose of this form is to demonstrate medical justification for prescribing the drug in question when. Ordering care providers will complete the notificationprior authorization process online or over the phone.
UnitedHealthcare Community Plan 112811 Louisiana Prior Authorization Fax Request Form 877-271-6290 Please complete all fields on the form and refer to the listing of services that require authorization. UnitedHealthcare Community Plan of New York UnitedHealthcare Community Plan Prior Authorization New York - Effective July 1 2021 Opens in a new window open_in_new FAQs. They will provide us with the information needed.
Prior Authorization Review is the process of reviewing certain medical surgical and behavioral health services according to established criteria or guidelines to ensure medical necessity and appropriateness of care are met prior to services being rendered. View our updated HIPAA information for UnitedHealthcare Community Plan. Member - ePA simplifies the prior authorization process ultimately getting members the medications they need faster minimizing disruption to therapy.
You may need approval or permission to get some services under the QUEST Integration plan. Plans supported include UnitedHealthcare Dual Complete and UnitedHealthcare Community Plan of Michigan and Healthy Michigan Plan. This is called prior authorizationYour doctor is responsible for getting a prior authorizationThey will provide us with the information needed.
UnitedHealthcare Community Plan Prior Authorization Requirements Michigan Medicaid Healthy Michigan Plan HMP and Childrens Special Health Care Services CSHCS - Effective June 1 2021. Your doctor is responsible for getting a prior authorization. Dedicated MLTSS IntakePrior Authorization number is.
Current Prior Authorization Plan Requirements UnitedHealthcare Community Plan of Michigan. Community Plan Pharmacy Prior Authorization For. Box 31365 Salt Lake City UT 84131-0365 Payer ID.
These authorizations are managed by UnitedHealth Clinical Services. This number continues to grow. Maryland Michigan Missouri New York Tennessee and Texas.
In some cases a physician may choose to prescribe medication that is not on the preferred drug list PDL and will have to fill out a UnitedHealthcare prior authorization form. Enrollment in the plan depends on the plans contract renewal with Medicare. Supported plans include UnitedHealthcare Dual Complete RP Regional PPO SNP R1548-001 and UnitedHealthcare Dual Complete HMO SNP H5253-041.
UnitedHealthcare Community Plan QUEST Integration PO. The Complete Prior Authorization List for Medicaid and MLTSS is available under the Billing Reference Guides Tab at.
Https Www Uhcprovider Com Content Dam Provider Docs Public Commplan Ky Forms Ky Medicaid Mco Prior Auth Form Pdf

Uhc Community Plans New Referral Program For 2021 Specialists Medical Coding Training Medical Coding Referrals

Aetna Medical Advantage Plans In Nc Sc And Tn For 2021 Medical Coding Training Medicare Advantage Medical Coding
Drug Lists And Pharmacy Uhcprovider Com

New York Providers And The New Bcbs Provider Network For 2021 In 2021 Networking Medical Coding How To Plan
Https Www Uhcprovider Com Content Dam Provider Docs Public Health Plans Dsnp Qrg 2021 Dsnp Qrg Hi R3175 003 000 Pdf

Figure 2a Healthcare Quarterly 21 3 Exploring Spatial Variation In Registration For Deceased Organ Donation In Ontario Canada Organ Donation Spatial Ontario

Clinical Research Coordinator Resume Objectives That Are Effective Job Resume Samples Clinical Research Project Manager Resume

Pin On Charts Graphs And Figures

The Center For Health Affairs Healthcare Business Healthcare Industry Affair

Aetna Medical Advantage Plans In Nc Sc And Tn For 2021 Medical Coding Training Medicare Advantage Medical Coding
Https Www Uhcprovider Com Content Dam Provider Docs Public Policies Medicaid Comm Plan Gender Dysphoria Treatment Cs Pdf

Uhc Community Plans New Referral Program For 2021 Specialists Medical Coding Training Medical Coding Referrals
Https Www Uhcprovider Com Content Dam Provider Docs Public Policies Medicaid Comm Plan Reimbursement Uhccp Consultation Services Policy R0129 Pdf

The Empire Plan Expands Use Of Unitedhealthcare Network Uhcprovider Com
Https Www Uhcprovider Com Content Dam Provider Docs Public Commplan Mi Forms Mi Uhccp Claim Reconsideration Form Pdf
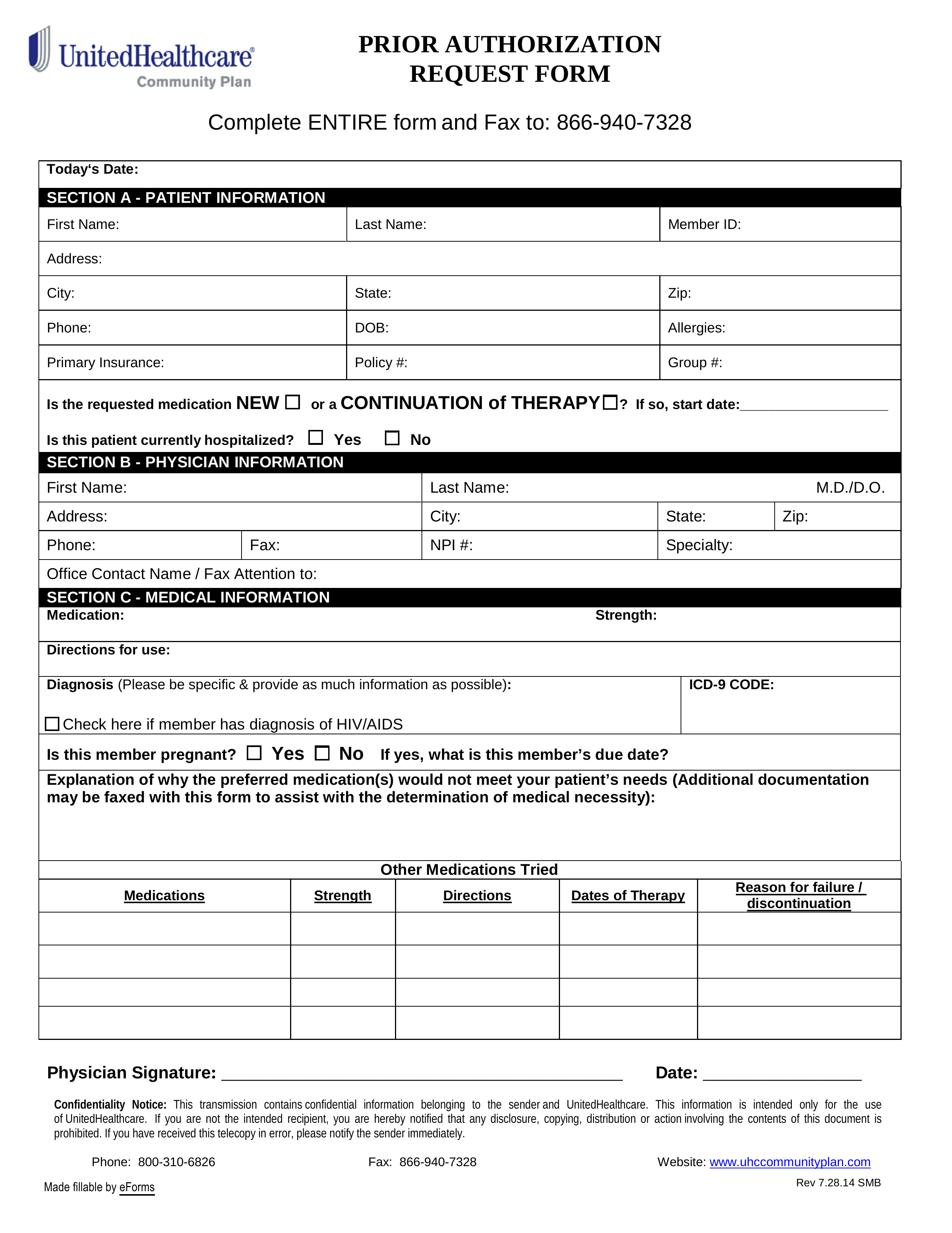
Free Unitedhealthcare Prior Rx Authorization Form Pdf Eforms
Https Www Uhcprovider Com Content Dam Provider Docs Public Commplan Mi Forms Mi Uhccp Claim Reconsideration Form Pdf

Virginia Medicaid Health Plans Unitedhealthcare Community Plan Medicare Medicaid Health Plans

Post a Comment for "United Health Care Community Plan Prior Authorization"